I believe in transparency.
Something I wasn't aware of when I first started looking for a therapist was the differences in payment options for therapy and how they worked. Don't worry if you've been confused-it's NOT just you! I firmly believe people should be given full transparency around their options so that they can make informed decisions for themselves. This guide will help you evaluate your options!
Individual 55-minute Session Rate: $150
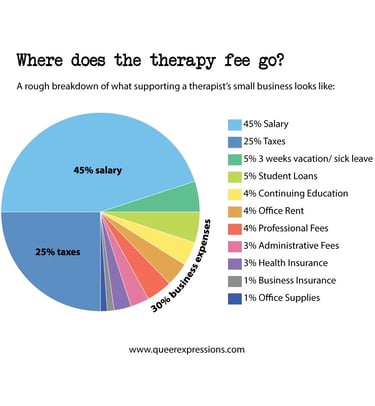
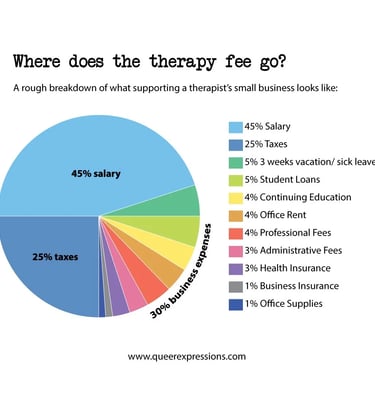
If you're interested, here's a blog post from another therapist, which offers an often-overlooked breakdown of why therapy is so expensive and why therapists may choose not to accept insurance.
Note: I am committed to making my practice as accessible as possible and offer a limited number of sliding-scale spots for those facing financial barriers. These are reserved for individuals with low household incomes, limited financial safety nets, or those who are unable to use insurance. If your current circumstances make my rates a barrier to care, please reach out—I’m happy to discuss how we can make this work for you.
This essentially is the "Pay and Get Reimbursed" Option.
This is the most common and often best option if you have a certain type of plan (usually a PPO or POS plan). It allows you to choose your therapist while getting reimbursed for a portion of the cost.
How It Works:
You Pay Upfront: You pay the therapist their full fee at the time of each session (this is called "out-of-pocket").
Superbill: Your therapist provides you with a special, detailed receipt called a Superbill (usually monthly). This is not a regular receipt; it has specific codes and information the insurance company needs, including:
Diagnosis Code (why you are being seen, e.g., Anxiety, PTSD).
Procedure Code (what service was provided, e.g., 60-minute therapy session).
The therapist's credentials and tax ID.
Submit a Claim: You submit this Superbill directly to your insurance company (usually through an online portal or by mail).
Reimbursement: If you have met your plan's Out-of-Network Deductible (a set amount you must pay before coverage kicks in), the insurance company will mail you a check for a percentage of the session cost (this is called Coinsurance).
Some insurance companies determine an “allowed amount,” which caps the session fee that they’ll cover. If your insurance has determined $100 is their “allowed amount” per session, at a 25% coinsurance rate, your insurance company will still only reimburse you up to $75, regardless of the therapist’s session fees. In other words, if your insurance has an allowed amount of $100 but your therapist’s session fees are $150 per session, you won’t get reimbursed more; you’ll still be reimbursed $75, and will be ultimately responsible for $75.
Guide on submitting claims for out-of-network benefits: https://blog.zencare.co/guide-to-out-of-network-benefits/.
Private pay:
This is essentially the "Self-Pay" Option.
This is the simplest way to pay and requires no additional work on your part.
How It Works:
You Pay Upfront: You pay the therapist their full, agreed-upon fee at the time of each session.
No Reimbursement: You do not submit any claims to your insurance company and receive no money back.
Advantages (aka why someone would choose this):
Privacy: This gives you maximum privacy, as your therapist does not need to submit a diagnosis or session notes to the insurance company, allowing you and your therapist more control over the treatment plan.
Clarity: There are no complex claims, denials, or surprise bills—you know exactly what you owe every time.
I am not in-network with insurance companies.
Here's why and your options:
Why are you out-of-network?
FSA/HSA (Flexible and Health Savings Accounts):
Using Tax-Advantaged Accounts
If you have a Flexible Spending Account (FSA) or a Health Savings Account (HSA), you can use these funds to pay for therapy, regardless of whether your therapist is in-network or out-of-network.
With this option (if not combined with using out-of-network benefits), you don't have to submit anything to your insurance company. However, you may need to submit detailed receipts (or the Superbill; Note: I have these records on your behalf) in case the FSA/HSA administrator or the IRS asks for proof that the expense was "medically necessary."
How It Works:
Pre-Tax Dollars: These accounts allow you to set aside money from your paycheck before taxes are taken out.
Payment: You can use a dedicated debit card (often provided by the account) to pay the therapist directly.
Savings: Since you are using pre-tax money, you effectively save money on your therapy costs equivalent to your income tax rate.
There are several reasons I chose to be out-of-network (meaning I don't have a contract with health insurance companies). The bottom line is that I choose to operate as an Out-of-Network (OON) provider because it allows me to prioritize your treatment needs above all else. While I accepted insurance for a long time, I stopped seeing the benefits for therapists and clients after health insurance companies made changes that put restrictions on client sessions and diagnostic requirements. Being OON allows me and my clients to maintain autonomy over their treatment, rather than having their insurance company dictate their treatment and what the insurance provider deems "medically necessary." For complex issues like trauma, deeper, flexible work is often needed. Being OON ensures that we maintain full autonomy and privacy over your care. We can determine the appropriate session frequency and length based solely on your progress, allowing me to provide the highest quality, individualized, and uninterrupted care you deserve.
Out-of-Network:
If you plan on using Out-of-Network Benefits:
Helpful questions to ask your insurance provider before starting therapy:
Do I have out-of-network benefits for outpatient mental health? (Outpatient means treatment outside a hospital, such as therapy sessions.)
What is my out-of-network deductible for outpatient mental health?
Once that deductible is met, what percentage will be reimbursed? (another way to ask: What is my out-of-network coinsurance for outpatient mental health?)
How many visits am I allowed per calendar year (is there is a restriction if I use my OON benefits)?
Do I need a referral from an in-network provider to see a therapist out-of-network?
How do I submit claim forms for out-of-network reimbursement? (Claims are forms that are sent to your insurance company to receive reimbursement for sessions you paid for out of pocket.)
What is my deductible, and has it been met?
Note: You can also look this information up yourself in the Summary of Benefits or Explanation of Benefits document.
For more information: https://blog.zencare.co/guide-to-out-of-network-benefits/
